Do you know what happens to your blood pressure while you sleep?
Most people check their blood pressure during the day. However, blood pressure changes at night can reveal critical, hidden health risks. This guide explains the crucial differences between nocturnal blood pressure monitoring and ambulatory blood pressure monitoring, highlighting their significance based on recent clinical research.
What Is Nocturnal Blood Pressure Monitoring?
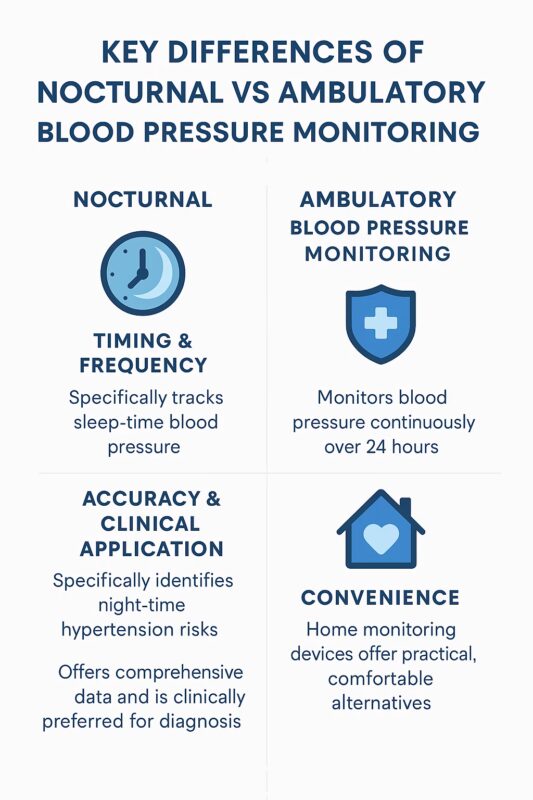
Nocturnal blood pressure monitoring specifically measures your blood pressure while you sleep. Doctors use this to assess how effectively your body regulates blood pressure overnight. Normally, blood pressure decreases by 10% to 20% during sleep a pattern known as nocturnal dipping.
Why Blood Pressure Drops at Night (or Doesn’t)
During sleep, your heart rate slows, and blood pressure naturally drops, allowing your cardiovascular system to recover. If your blood pressure does not fall sufficiently, your heart continues working hard even during rest, increasing the risk of heart disease and stroke.
The “Non-Dipper” Effect and Cardiovascular Risk
Some individuals are “non-dippers”, meaning their blood pressure does not adequately decline at night. Clinical studies reveal non-dippers face nearly twice the risk of cardiovascular events compared to those with normal dipping patterns, alongside increased risks of stroke, kidney problems, and other complications.
Visual Example of Blood Pressure Dipping Patterns
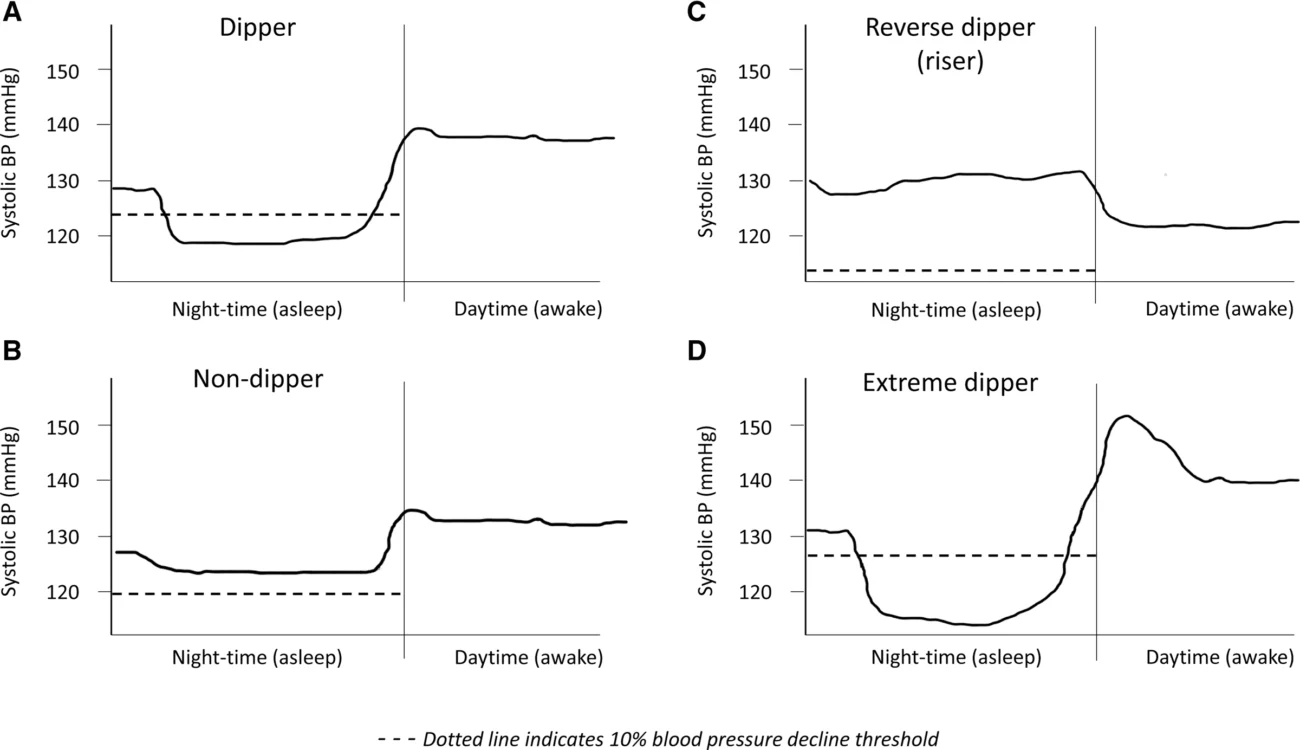
How Nocturnal Readings Help Catch Hidden Hypertension
Night-time monitoring can reveal “masked hypertension” high blood pressure that appears normal during daytime surgery or clinic visits. Research strongly suggests nocturnal monitoring improves early detection, facilitating earlier and more effective treatment strategies.
What Is Ambulatory Blood Pressure Monitoring (ABPM)?
Ambulatory blood pressure monitoring (ABPM) records your blood pressure over a full 24-hour period using a portable device. Typically, it measures every 15-30 minutes, providing a comprehensive profile of how your blood pressure changes throughout daily activities and sleep.
What Does ABPM Involve?
You wear a small, portable monitor attached to a cuff around your upper arm. It automatically inflates periodically, capturing accurate blood pressure data during your usual routines and whilst you sleep. After 24 hours, your GP or clinician analyses the detailed readings.
24-Hour Monitoring vs. Office-Based Readings
Research confirms ABPM provides superior accuracy compared to traditional surgery-based readings. It effectively identifies “white coat hypertension” (blood pressure elevated only in clinical settings due to stress) and masked hypertension, offering a robust prediction of cardiovascular risk.
The Key Differences Between Nocturnal vs Ambulatory
Who Needs ABPM and When?
Doctors recommend ABPM in the following cases:
- Unclear or elevated surgery-based blood pressure readings
- Suspected white coat or masked hypertension
- Significant blood pressure variations during daily activities
- Adjusting or evaluating treatment effectiveness
ABPM helps doctors create better treatment plans based on your full 24-hour profile.
Home Monitoring Solutions That Bridge the Gap
Traditional ABPM devices can be uncomfortable, especially during sleep. Modern home solutions, such as the Aspedan Bluetooth Blood Pressure Monitor, enable convenient and accurate monitoring without continuous wear.
How Smart Devices Help Replicate ABPM Results
The Aspedan Bluetooth Blood Pressure Monitor supports regular morning and evening readings, effectively capturing important patterns similar to ABPM. Regular tracking over weeks provides clinically meaningful insights into night-time blood pressure trends and daily fluctuations.
Using Aspedan to Track Morning and Evening Readings
Aspedan’s health tracker app helps you log your readings easily. You take a reading after waking up and before sleeping. The app stores the data, helping you and your doctor see how your blood pressure behaves. This routine can reveal problems like morning hypertension or non-dipping at night.
Real-Time Data, Clinician Reports, and Long-Term Trends
The Aspedan monitor syncs data through Bluetooth. You can share your results with doctors directly from the app. The system also shows long-term trends, helping you understand how your lifestyle, stress, or medication affects your blood pressure. This allows for quick action if your readings change.
Sleep Quality, Disorders, and Blood Pressure
Good quality sleep is essential for healthy blood pressure patterns. Obstructive sleep apnoea (OSA) is a significant contributor to nocturnal hypertension, causing frequent surges in blood pressure during sleep. The link is bidirectional: those with OSA are more likely to have hypertension, and people with hypertension are more likely to have OSA.
Disrupted or poor-quality sleep whether due to OSA, insomnia, or lifestyle factors can prevent the expected nocturnal dip, raising cardiovascular risk. Treatment of OSA, for example with continuous positive airway pressure (CPAP), can reduce night-time blood pressure and improve outcomes. Addressing sleep hygiene, managing stress, and diagnosing sleep disorders are vital steps in long-term blood pressure control.
Chronotherapy and Medication Timing
Recent studies suggest that the timing of blood pressure medication can impact its effectiveness, particularly for controlling nocturnal hypertension. Taking at least one antihypertensive tablet at bedtime, rather than in the morning, may offer better control of night-time blood pressure and help restore the natural dipping pattern. However, medication timing should always be discussed with your GP or consultant, as research continues and individual factors may influence what is best for you.
Limitations and Practical Considerations
While ABPM is considered the gold standard for diagnosing hypertension and assessing nocturnal blood pressure, it can be uncomfortable and is not always widely available. Night-time readings can sometimes be affected by sleep disturbance from the device itself. Defining “night-time” also varies some methods use fixed time periods, others rely on patient self-report or actigraphy. Each approach has benefits and drawbacks, but for most people, self-reporting sleep and wake times is reliable.
Practical Tips for Better Blood Pressure Monitoring
- Maintain a sleep diary if using ABPM or home monitoring.
- Prioritise good sleep hygiene and treat any sleep disorders, such as OSA.
- Share your readings with your GP or healthcare provider for regular review.
- Use validated home devices, especially if regular night-time readings are needed.
Future Directions: Personalised and Connected Monitoring
Personalised hypertension management is becoming more feasible with advances in wearable technology and artificial intelligence. Continuous, minimally disruptive blood pressure monitoring both day and night will allow earlier detection of abnormal patterns and more precise, proactive treatment.
Final Thoughts
Blood pressure monitoring helps you stay in control of your health. You can choose Nocturnal vs Ambulatory, or home monitoring based on your needs. Talk to your doctor to select the best option. Reliable home devices like the Aspedan Bluetooth Blood Pressure Monitor allow you to collect accurate data at home. With daily readings, clear reports, and smart app features, Aspedan supports your long-term health goals. You get simple tracking, easy data sharing, and full control over your blood pressure management.
References
- European Cardiology Review: The Role of Nocturnal Blood Pressure and Sleep Quality in Hypertension Management
- PMC: Differences in Nighttime and Daytime Ambulatory Blood Pressure When Diurnal Periods Are Defined by Self-report, Fixed-Times and Actigraphy
- Hermida RC et al., Eur Heart J, 2020
- Hansen TW et al., Hypertension, 2021
- Parati G et al., JAMA Cardiology, 2022